We dare to advance palliative care

“Don’t add to the confusion. Palliative care and end of life are not synonymous.”
Confronting that confusion is an objective for the faculty members on the informally assembled but intensely dedicated Palliative Care Team at the University of Michigan School of Nursing. Clinical Assistant Professors Karen Harden, DNP, MS, RN, AOCNS, Deb Price, DNP, MS, RN, and Heidi Mason, RN, DNP, ACNP-BC, along with Clinical Associate Professor April Bigelow, Ph.D., ANP-BC, AGPCNP-BC, have integrated their efforts to improve palliative care education and lead new conversations about the future of the field.
Building a better understanding of palliative care
In 2014, Price began research on palliative care competencies in different health disciplines. Her study of 22 units at Michigan Medicine resulted in four publications, which demonstrated clinical and communicative gaps in palliative care practice as well as the need for palliative care education among nurses and other health care professionals.
“While the focus is on quality of life and symptom management, palliative care can happen along with concurrent care throughout the course of one’s illness,” she explained. “Palliative care conversations should start at the beginning of the diagnosis of any life-limiting illness; they should start in the outpatient setting so patients can discuss what’s important to them.
“It’s about re-educating everyone across the system and getting all of the disciplines together. Everyone has strengths that can provide better support to patients and families.”
The four faculty clinicians have practiced and researched palliative care in different capacities throughout their careers. Last year, when Bigelow began a Hospice and Palliative Medicine Fellowship at Michigan Medicine, the group started meeting together and adopted the Palliative Care Team moniker. Together, their work extends from the hospital and clinic into the community and classroom.
“We all could still be working in silos in our own research if we hadn’t started talking to one another,” said Harden. “Informally, we brought ourselves together and realized if we consolidate what we’re doing, we can all benefit.”
Exploring the effects of the pandemic
 In conjunction with an educational mission, the team is using their collective expertise to spark new discussions around current issues in the field, including those brought to light by COVID-19.
In conjunction with an educational mission, the team is using their collective expertise to spark new discussions around current issues in the field, including those brought to light by COVID-19.
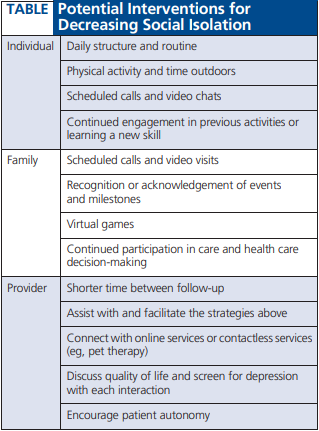
In December, a paper co-authored by the four faculty members will be published in The Journal of Hospice and Palliative Nursing. "COVID-19 Shines a Spotlight on the Age-old Problem of Social Isolation," examines the wide-ranging effects of social isolation in hospital, ambulatory care and assisted living settings. Using three case studies, the publication sets forward themes and challenges the pandemic has presented to patients, families and providers while also discussing possible interventions.
“The potential long-term implications of people who were infected, including the mental health impact, will be driving additional palliative care interventions,” said Bigelow. “This underscores the need for more palliative care education, because there is a shortage of people who have the right skill set. In order to provide the best care, we need to develop programs that can teach people how to interact with patients and families.”
The team has also received an exploratory grant to investigate palliative care competencies in primary care providers. Bigelow and Mason are lead investigators on the research, which will survey primary care physicians, nurse practitioners and physician assistants across the country.
“Primary care providers in particular are going to see a greater need for palliative care skills as their patients may be dealing with issues related to the pandemic,” Bigelow said. “We want to determine their baseline knowledge so we can help them integrate palliative care concepts into their daily practice.”
Education is essential
For the last few years, Palliative Care Team members have coordinated two large-scale events and a number of other educational initiatives.
The Nursing Core Curriculum is a one-day basic skills event specifically for nurses that teaches essential palliative care competencies over the course of an intensive 8-hour program. The first session was held in 2019 with more than 100 participants, and plans are now underway for a virtual session in spring 2021.
The Power of Palliative Care Conference brought more than 150 professionals to The School of Nursing in 2017 and 2018. The two-day event focuses on palliative care basics for interdisciplinary practice, including topics like end-of-life conversations, complex family dynamics and symptom management. This year’s conference centers on lessons learned from COVID-19 and will take place as a free webinar on Wednesday, Sept. 16, from 8 a.m. to noon. Students, faculty, staff and any interested attendees can join the conference on Zoom to view real-time presentations and a panel discussion with members of the Palliative Care Team, specialists from Michigan Medicine and other experts in the field.
“One good thing about all of the virtual learning is it has increased access for many people, so some of those who may not have been able to travel to campus now have access to these events through a new platform,” said Harden.
Key to the Palliative Care Team’s efforts is a collaborative relationship with Michigan Medicine. Team members regularly partner with the health system’s Palliative Care Providers group, and Price serves as co-chair of the hospital’s Palliative Care Education Committee.
Mason has developed an in-depth palliative care education program for nurse practitioners and physician assistants at the U-M Rogel Cancer Center. The professional development program, like many courses across campus, has shifted to a virtual format, which kicks off in September with the first of eight sessions focusing on the different domains of palliative care.
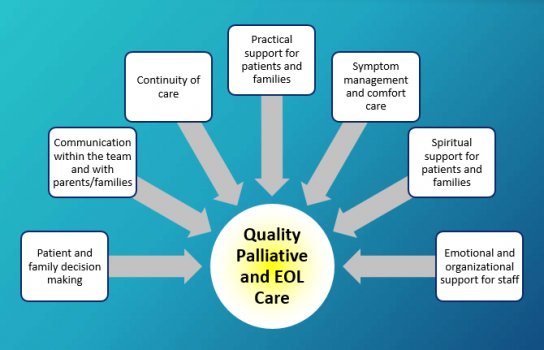
“These programs focus more on concrete strategies for providers to implement in their daily work. Things like when to identify, when to refer for treatment and other basic palliative care skills,” Mason explained.
For the last two years, Harden has been a member of Michigan Medicine’s IPEX group, a nursing, medicine, pharmacy, social work and spiritual care collaborative that has been developing a program to educate learners of all disciplines at the hospital’s inpatient Department of Palliative Care. The group has created a learning module in palliative care and interprofessional collaboration, and is now testing to evaluate its effectiveness.
Team members have also been focused on how to integrate palliative care into the curriculum at the School of Nursing. Each winter, Harden and Mason lead a palliative care elective course that brings graduate and undergraduate nursing students together. The course uses internationally recognized palliative care modules and features guest lectures from physicians, pharmacists, social workers and experts in complementary therapies.
“Our curriculum looks at the whole patient, where they came from and where they’re going,” said Price. “Understanding that helps you understand how to help them the most, and that’s really what palliative care is all about.”
More work to do
Price and her colleagues are quick to admit that while palliative care has progressed, there is still a long way to go.
“Recognizing the need for palliative care has only been around for about 18 to 19 years,” she said. “We have to educate everyone in primary palliative care, to recognize when suffering is happening and the conversations that need to occur — and everybody can do that.”
While much work remains, the faculty experts who form U-M School of Nursing’s Palliative Care Team are motivated by a shared mission to magnify the impact of a clinical practice that’s too often misunderstood.





