Main Menu
- About
- News and Publications
- Events
- Dean Patricia D. Hurn
- Visit us
- Contact us
- Facilities and Safety
- Departments
- Operations teams
- Data and dashboards
- Healthcare Innovation Impact Program (HiiP)
- Sharing Your Ideas & Innovations
- Advancing a Culture of Innovation
- The Innovator Pathway
- Supporting Our Innovators
- Building Innovation Bridges
- Building Student Engagement
- Innovate 4 Change
- Resources and Funding
- Innovation Webinars & Podcasts
- HiiP Innovation Fellows
- HiiP Innovations in the News
- Contact HiiP
- 2024 HiiP Innovation Week
- Rankings
- Tech support
- History of our School
- Mission and Vision
- Sexual Misconduct & Harassment Resources
- Academics
- Bachelor of Science in Nursing (BSN)
- Master of Science in Nursing (MSN)
- Doctor of Nursing Practice (DNP)
- Doctor of Philosophy in Nursing (Ph.D.)
- Specialties
- Adult-Gerontology Acute Care Nurse Practitioner
- Adult-Gerontology Primary Care Nurse Practitioner
- Nurse-midwifery
- Nurse-midwifery and Primary Care Family Nurse Practitioner (Combined)
- Primary Care Family Nurse Practitioner
- Primary Care Pediatric Nurse Practitioner
- Leadership, Analytics and Innovation
- Post-master's DNP
- Concentrations
- Certificates
- Accreditations & Disclosures
- Clinical Learning Center (CLC)
- Clinical placements
- Nursing courses
- Digital Education
- Admissions and aid
- Research
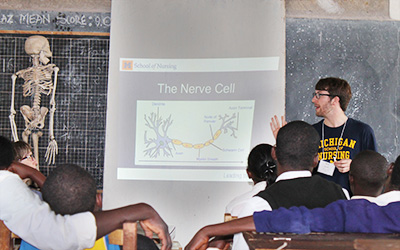
- Global
- Diversity
- Alumni
- Giving